Track: Hot Topics
Poster : COVID-19
Kara N. Goldman
Assistant Professor, Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility
Northwestern University
Chicago, Illinois
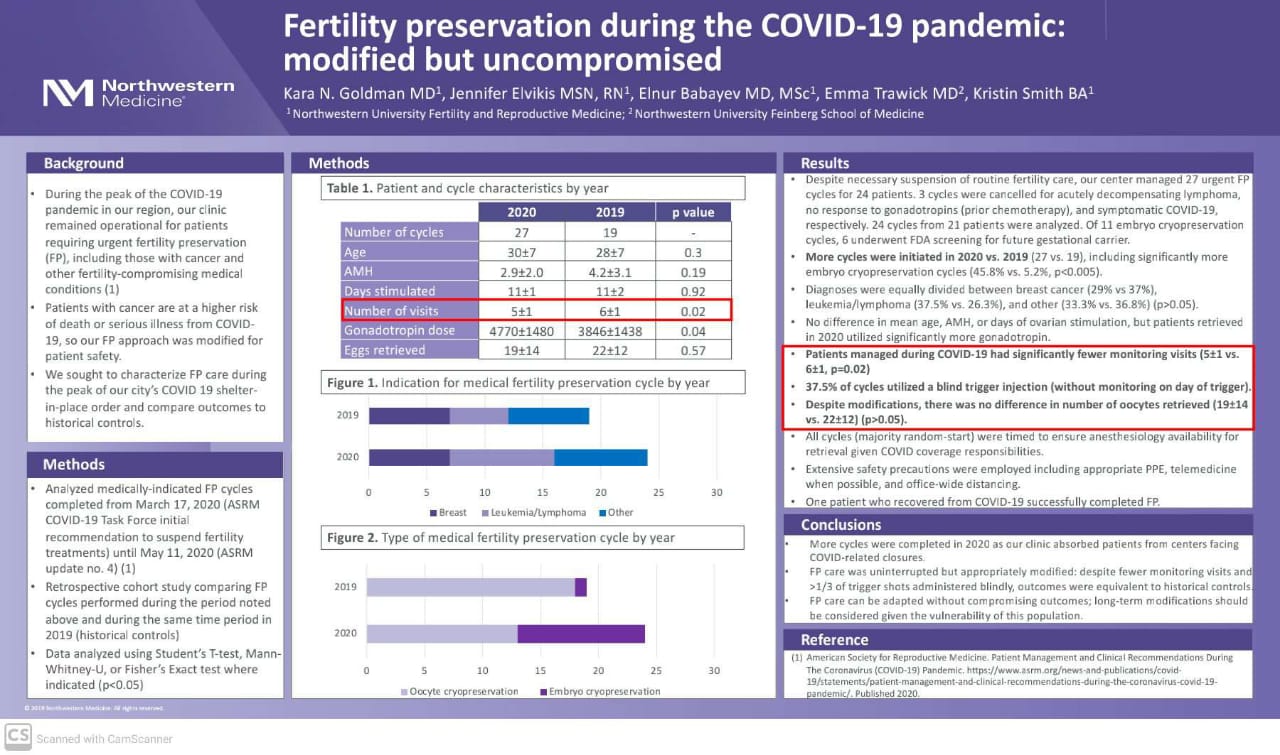
Objective: During the peak of the COVID-19 pandemic, our clinic remained operational for patients with cancer and other fertility-compromising medical conditions requiring urgent fertility preservation (FP). As patients with cancer are at a higher risk of death or serious illness from COVID-19, our FP approach was modified for patient safety. We sought to characterize FP care during the peak of our city’s COVID-19 shelter-in-place order and compare outcomes to historical controls. DESIGN: Retrospective cohort study with historical controls MATERIALS AND
Methods: We analyzed all medically-indicated FP cycles completed from March 17, 2020 (ASRM COVID-19 Task Force initial recommendation to suspend fertility treatments) until May 11, 2020 (ASRM update no. 4). Cycles performed during the same time period in 2019 were compared as historical controls. Data were analyzed using student’s T-test, Mann-Whitney-U, or Fisher’s Exact test where indicated (p<0.05).
Results: Despite suspension of routine fertility care, our center managed 27 urgent FP cycles for 24 patients. 3 cycles were cancelled for acutely decompensating lymphoma, no response to gonadotropins (prior chemotherapy), and symptomatic COVID-19, respectively. 24 cycles from 21 patients were analyzed. Of 11 embryo cryopreservation cycles, 6 underwent FDA screening for future gestational carrier. More cycles were initiated in 2020 vs. 2019 (27 vs. 19), including significantly more embryo cryopreservation cycles (45.8% vs. 5.2%, p<0.005). Diagnoses were equally divided between breast cancer (29% vs 37%), leukemia/lymphoma (37.5% vs. 26.3%), and other (33.3% vs. 36.8%) (p>0.05). There was no difference in mean age (30 ±7 vs 28 ±7), AMH (2.9±2.0 vs. 4.2±3.1), or days of ovarian stimulation (11±1 vs. 11±2) (p>0.05) but patients retrieved in 2020 utilized significantly more gonadotropin (4770±1480 vs. 3846±1438, p=0.04). Notably, patients managed during COVID-19 had significantly fewer monitoring visits (5±1 vs. 6±1, p=0.02), and 37.5% of cycles utilized a blind trigger injection (without monitoring). Despite modifications, there was no difference in no. of oocytes retrieved (19±14 vs. 22±12) (p>0.05). All cycles (majority random-start) were timed to ensure anesthesiology availability for retrieval given COVID coverage responsibilities. Extensive safety precautions were employed including appropriate personal protective equipment, telemedicine when possible, and office-wide social distancing. One patient who recovered from COVID-19 successfully and safely completed FP.
Conclusions: At our center FP care remained uninterrupted but appropriately modified during COVID-19. We completed more cycles compared to 2019, absorbing patients from centers facing COVID-related closures. Despite significantly fewer monitoring visits and more than one-third of trigger shots administered blindly, outcomes were optimal and equivalent to historical controls. Our center’s experience illustrates that FP care can be adapted without compromising outcomes; long-term modifications should be considered given the continued vulnerability of this population.
ASMR official sponsorship in the publications of the virtual ASMR conference October 17-21 October 2020