Track: ART – LAB
Poster : ART Lab: Basic
Albert Li
Embryologist
Reproductive Medicine
Associates of New York
New York, New York
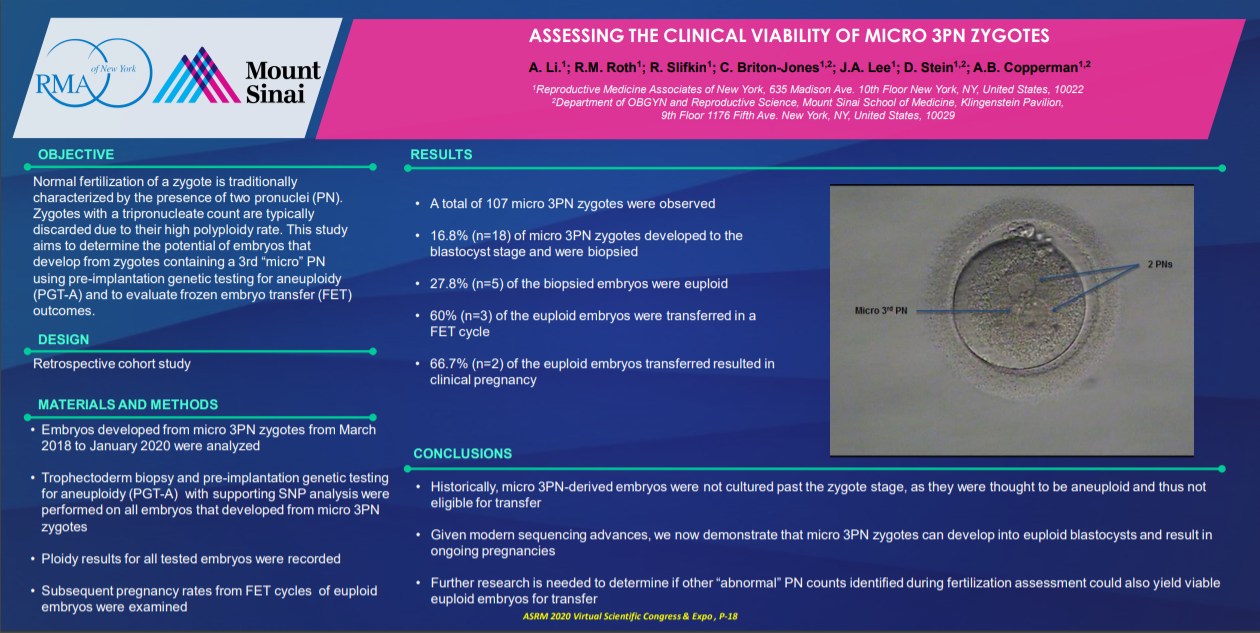
Objective: Following intracytoplasmic sperm injection (ICSI) of an oocyte in vitro, fertilization is evaluated using morphological assessment and count of pronuclei (PN). Normal fertilization is characterized by the appearance of 2 PN, observed 13-19 hours post-ICSI. Occasionally, a 3rd “micro” PN can be observed in the zygote. This finding has traditionally been interpreted by embryologists to be an abnormality that is consistent with embryonic aneuploidy, including triploidy [1,4]. Reproductive biologists have demonstrated that the appearance of a 3rd micro PN following injection of a single spermatozoon can result from the retention of the second polar body, oocyte meiotic failure, or sperm abnormalities [2, 3]. Embryos resulting from tri-pronucleated zygotes have also been found to be euploid, perhaps due to self-correction during subsequent cell division [4]. This study aims to evaluate the clinical viability of micro 3PN zygotes by assessing rates of embryo ploidy and frozen embryo transfer (FET) outcomes. DESIGN: Retrospective MATERIALS AND
Methods: Micro 3PN zygotes were identified from patients who underwent IVF with ICSI and pre-implantation genetic testing for aneuploidy (PGT-A). On day 3 of development, embryos underwent laser assisted hatching to breach the zona pellucida. At the blastocyst stage of development (day 5, 6 or 7), a trophectoderm biopsy was performed on any embryo(s) that met biopsy criteria (≥5 trophectoderm cells herniating, ≥grade “C” inner cell mass and trophectoderm). Samples of biopsied trophectoderm were sent to a commercial laboratory for genetic analysis using a next generation sequencing method. Embryos were vitrified post-biopsy, and euploid embryos were subsequently thawed for FET.
Results: A total of 107 micro 3PN zygotes were evaluated between March 2018 and January 2020. After culturing to the blastocyst stage,16.8% (n=18) of the embryos were biopsied, and 72.2% (n=13) of those displayed diverse types of aneuploidy, although triploid embryos were not found. A euploid rate of 27.8% (n=5) was detected, with 60% (n=3) of those transferred in a FET cycle. A clinical pregnancy rate of 66.7% (n=2) was achieved. One patient reported a livebirth and the other pregnancy is currently ongoing.
Conclusions: This study demonstrates the reproductive potential of micro 3PN zygotes within an IVF setting. Although there is a high rate of embryonic aneuploidy in micro 3PN-derived blastocysts, our study shows a proportion of these embryos are euploid, can be selected for embryo transfer, and lead to a positive pregnancy outcome. We suggest extending culture of micro 3PN zygotes due to their capability of having a normal genetic profile. With the validation of genetic screening, patients can be assured that normal pregnancies can be sourced from micro 3PN zygotes.
ASMR official sponsorship in the publications of the virtual ASMR conference October 17-21 October 2020