Track: Health Disparities
Poster : Health Disparities
Zachary Walker
Resident
University of Alabama at Birmingham
Birmingham, Alabama
Objective: To assess the relationship between different racial-ethnic groups and rates of abnormal semen analysis (SA). DESIGN: Retrospective cohort study MATERIALS AND
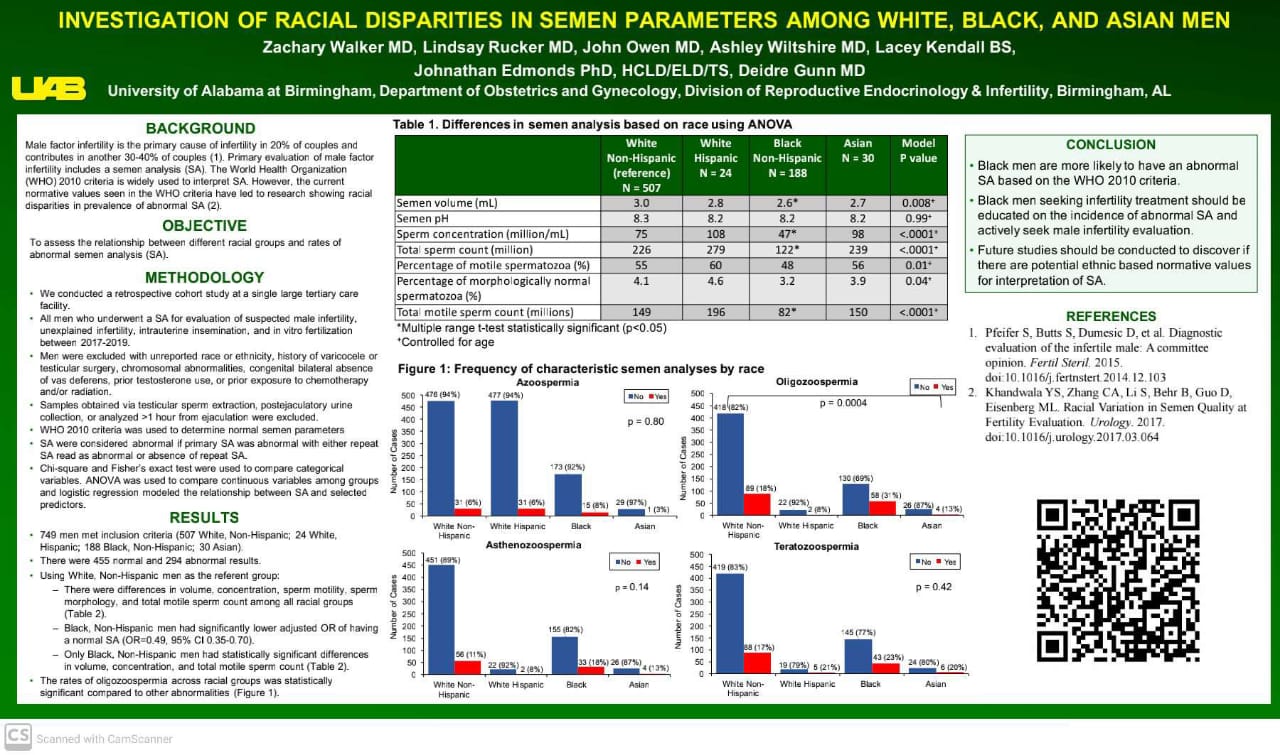
Methods: All men who underwent a SA between January 1, 2017 and December 31, 2019 at a single tertiary care center were considered for the study sample. Those with an unknown race-ethnicity, varicocele, history of testicular surgery (e.g., varicocelectomy, vasectomy, or vasectomy reversal), genetic anomalies, congenital absence of bilateral vas deferens, prior testosterone use, or prior exposure to chemotherapy/radiation were excluded. Samples obtained via testicular sperm extraction, postejaculatory urine, or analyzed >1 hour from being received were also excluded. The World Health Organization (WHO) 2010 criteria was used to determine normal semen parameters. If a second SA was interpreted as normal following an initial abnormal result, the result was considered normal for the analysis. Racial-ethnic groups comprised White, Black, Hispanic, and Asian. Chi-square and Fisher’s exact test were used to compare categorical variables. ANOVA was used to compare continuous variables among groups and logistic regression modeled the relationship between SA result and selected predictors.
Results: In total, 872 SAs were initially performed. Only 750 met inclusion criteria, yielding 456 Normal and 294 Abnormal results. Only Race-ethnicity (p<0.0001) and Age (p=0.003) were statistically significant in the baseline demographics. 54% of Black men had an abnormal semen analysis. Black men were more likely to have hypospermia, oligozoospermia, and lower total motile sperm counts (Table 1). In a logistic regression model, controlling for age and using White as the referent group, only Blacks had lower odds for a normal SA (OR=0.49, 95% CI 0.35, 0.70).
Conclusions: Black men are more likely to have an abnormal SA based on the WHO 2010 criteria. Black men seeking infertility treatment should be educated on the incidence of abnormal SA and actively seek male infertility evaluation. Future studies should be conducted to discover if there are potential ethnic based normative values for interpretation of SA. Table 1: Differences in Semen Analysis based on Race-Ethnicities using ANOVA

ASMR official sponsorship in the publications of the virtual ASMR conference October 17-21 October 2020